History of Anaplastic Large Cell Lymphoma
Breast Implant Associated- Anaplastic Large Cell Lymphoma (BIA-ALCL) is not a breast cancer. Breast implants have been in the news and I would like to offer a perspective. This is a rare highly treatable process that occurs approximately 8-10 years post implant whether saline or silicone, cosmetic or reconstructive procedure. Symptoms will appear as a delayed seroma, a sudden enlargement of a breast due to a fluid collection or a palpable mass. This only involves textured implants.
Overall incidence is 1:20,0000 or 0.005% risk, whereas the risk of breast cancer in a women’s lifetime is 12.5% or 1:8.
Recurrent Breast Cancer 5-8%
Capsular Contracture/10 years 14%
Implant Rupture/10 years 8%
Diagnosis of Anaplastic Large Cell Lymphoma
Diagnosis of a sudden breast enlargement should be evaluated. Usually an Ultrasound and aspiration of fluid for cytology(checking for cells); not all fluid collections are BIA-ALCL In the presence of a palpable mass tissue needs to be obtained for examination; for that reason it may just require a fine needle biopsy or if deeper a stereotactic needle or open biopsy.
Treatment
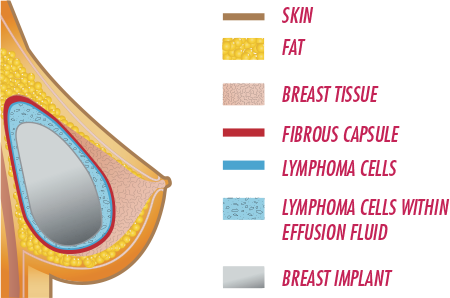
Treatment of Breast Implant Associated- Anaplastic Large Cell Lymphoma (BIA-ALCL)is to remove the implant and the capsule. Consequently the capsule is present in all patients and is merely the bodies response to the presence of the implant. Majority need no other therapy.
FDA does not recommend asymptomatic prophylactic removal, however, Allergan has been contacting patients in their registry who have textured implants and offering a swap to a smooth surfaced implant. https://www.plasticsurgery.org/patient-safety/breast-implant-safety/allergan-biocell-device-withdrawal. Unfortunately, they do not cover the surgeons, anesthesia or facility fee.
The science behind this disease is multifactorial including; genetic predisposition, texturing technique and subclinical bacterial infection with a biofilm formation. When a biofilm is present it triggers inflammation that leads to an immune response. Therefore the best practice to reduce formation of a biofilm is administration of an antibiotic pre-operatively, irrigation of the pocket with an antibiotic solution and a layered closure; as a result a process I have employed for nearly thirty years.